|
Cat Vet Care
in Gilbert AZ

|
|

|
|
CAT INFORMATION
Basics:
Animals can show similar signs of illness with many different diseases, but there are some signs of disease that are commonly seen especially in older cats or cats with specific diseases. As always, it is important to have your individual cat examined by your doctor and to follow his/her recommendations. The following discussion is intended to help you identify a few of the problems you may see in your cat and to discuss possible causes. Disease occurrence is often very specific to the patient’s age with seniors, adults and kittens all having their own unique set of problems. So, I’ve split the discussion into age related diseases for kittens, adults and seniors.
Kittens: for our purposes are less than 1 year old
Common Problems:
- Viruses
- Parasites – internal (worms) and external (mites)
In young animals viruses and parasites are the most common problem we encounter. The best way to protect your cat is to vaccinate early and completely. Many people don’t realize that, depending upon the cat’s age when first vaccinated; he or she will require at least one booster vaccine to actually become protected. Kittens will also commonly have worms that can potentially be infectious to children (rare) and we recommend that all young animals be treated for roundworms and hookworms to eliminate this risk. And ear mites are occasionally seen as thick clumps of brown debris in the ears. Ear mites are not infectious to people but can be transmitted to other kittens and puppies.
|
|

|
|
Common Signs of Illness:
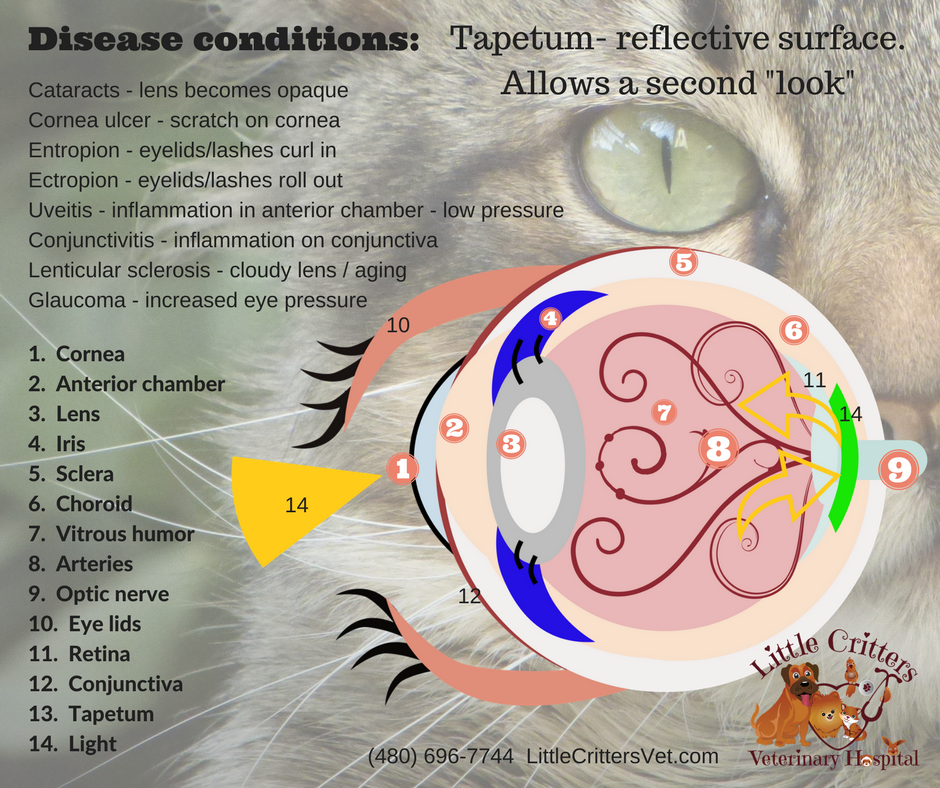
– Head Cold like signs and/or diarrhea Common signs of illness in kittens are often similar to a person with a head cold (although not an infection shared with humans) with sneezing, nasal discharge and runny eyes. Cats can actually become infected with several different types of upper respiratory infections (URI) and can cause signs similar to a head cold. Some of these URIs can also cause eye infections and corneal ulcers. Ulcers are an injury to the surface of the eye from the virus and can be very painful to the kitten. Typically the cat will squint and have tearing. If seen, this should always be addressed quickly to avoid further injury or rupture of the eye. Supportive care for the sick kitten often involves treating any eye infections, antibiotics for secondary bacterial infection (if indicated), fluids for dehydration and ensuring adequate food intake. Cats eat based on smell and with a stuffed up nose many kittens will have a decreased appetite. A good way around this is to keep the nose clean and warm up the food to bring out the smell.
Typical Vaccines:
May vary somewhat between hospitals and states
1) FVRCP: Protects from organisms that can cause respiratory infections as well as eye infections, vomiting and diarrhea. We will typically give the combined FVRCP vaccine every 3 weeks for a series of 3 visits.
- Calici Virus
- Chlamydia psittaci
- Feline Rhinotracheitis
- Panleukopenia virus
2) FELV: Protects from feline leukemia virus which causes immunosuppression and opportunistic infections and cancer. The leukemia vaccine is only given to cats with potential exposure to other cats. Typical transmission is via bite wounds or fighting. A booster is needed.
3) Rabies: Protects from Rabies virus Rabies is given once at the last kitten visit and repeated yearly or every 3 years based on state laws. Cats are one of the growing risk groups for rabies infection in the US. In part this is due to poor owner compliance with vaccination and also the cats are more likely to encounter infected wildlife such as bats.
Diarrhea: from parasites, viral infection or dietary changes
Another common problem in kittens is diarrhea. Diarrhea can occur from parasites, viruses and dietary change. We always recommend that you convert your new pet to any new diet slowly to avoid diarrhea. All kittens showing diarrhea should have a physical examination to check the kitten’s general health and also a fecal examination for potential parasitic infections. Most parasitic infections can be easily eliminated with the appropriate medications. However, many parasite infections require different types of medication, so you should always have a fecal exam done to identify the specific parasite which allows treatment with the appropriate medication.
Recommend deworming all kittens at least twice with a medication effective against roundworms and hookworms.
Additional Suggestions:
- New kittens should be tested for FELV/FIV (leukemia & feline immunodeficiency virus
- All new pets should have a microchip placed for permanent identification
- Flea and tick prevention may be needed depending upon the state of residency and potential exposure to the outdoors
Spay & Neuter:
All pets should be spayed or neutered to prevent unwanted pregnancies, reduce disease occurrence and help control roaming and urine marking. The age will vary with the hospital but typically we recommend sterilizing between 4-6 months of age
|
|

|
|
ADULTS:
Adult cats comprise the largest category and can have the most diverse illnesses based on their history, diet and environment. Typical signs of problems include: vomiting, trauma, skin abscesses, decreased appetite, straining to urinate, urine marking in the house, hiding or lethargy and many other potential signs can occur. Adult cats are usually more resistant to viruses (due to previous vaccines) and parasites, but we’ll see problems such as dental disease, urinary tract infections, organ disease, inflammatory bowel disease, allergies, behavioral issues, foreign bodies, ear and eye infections and much more. It is impossible to list all potential problems, so the safest course of action is to have your cat examined yearly by your veterinarian and certainly examined at the first sign of illness. Adults are often the forgotten group as we often just expect them to remain healthy. However, just as adult people can become ill, so can adult cats. The best recommendation I can give is to have a regular annual vet exam for all adults and so pay close attention to your pet’s normal behavior and activity. Frequently, the only sign of illness in a cat is a subtle change in behavior and perhaps less social interaction with more sleeping or hiding. This seems to be especially true for periodontal and urinary diseases.
|
 |
|
SENIORS:
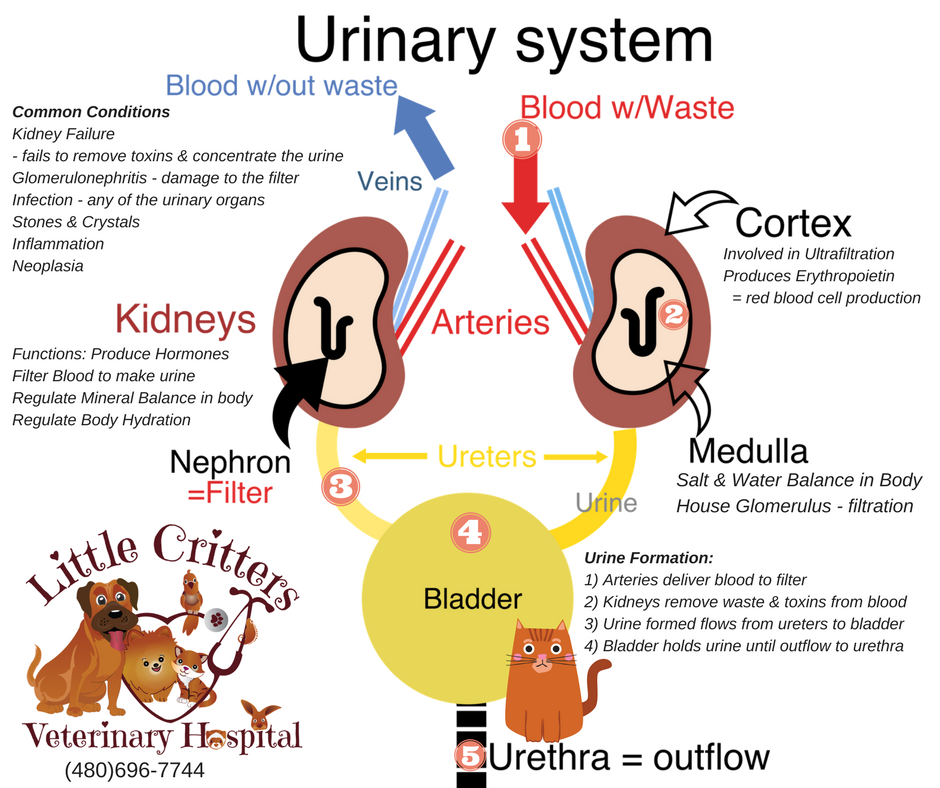
The age at which cats are considered seniors will vary from one doctor to another, but a good rule of thumb is to consider all cats at 10 years and older to be seniors. For senior pets it is always advisable to monitor their water intake and urine output. If you are suddenly seeing your kitty at the water bowl all the time, this may indicate a problem. Likewise, if your kitty has gone from making little puddles in the clumping litter to large lakes than the urine output is likely too high. Increased drinking and urination (pd/pu) is very common in cats with kidney disease, liver disease and diabetes. All of these diseases will often look very similar and therefore it is important that your veterinarian examine your cat and run blood work and urinalysis to check the organ status and the abilities of the kidneys to concentrate urine (retain fluid).
Four common diseases associated with aging in cats are:
- Kidney Failure: A loss of the cat’s ability to retain fluid, results in increased drinking and urination
- Diabetes Mellitus: Inability to regulate blood sugar, commonly causes increased drinking and urination with weight loss, more common in obese cats
- Hyperthyroidism: An over active thyroid which often causes weight loss in spite of a good to ravenous appetite.
- Neoplasia (cancer): Cancer can occur in animals of any age, but is more common in older pets. Many times there are few signs of illness but weight loss and problems specific to the site of the tumor may be seen.
Seniors should be examined by a veterinarian every 6-12 months and should have lab screening done yearly. Typical screening includes a complete blood and urine profile with a thyroid level.
Dental disease can also be a problem in older cats and many will require yearly dental cleaning. All types of dental disease occur in cats, but a common one at any age is called cervical line lesions. These are little craters formed in the teeth, often at the gum line, that result in inflammation and pain. Teeth with CLLs should be extracted. We’ll often also see tooth loss and abscess formation with pronounced dental disease. And finally, some cats develop a condition of severe inflammation (Gingivitis/Stomatitis) involving their gums and oral cavity and these pets must be medicated and treated aggressively to control their discomfort.
|
|
A five month old kitten who already has severe gingivitis and oral pain. Note the red gums around all the teeth. Preventative dental care is important with these patients and many will need to have their teeth extracted at some point to control the pain. The disease is thought to be associated with a over active immune system that is reacting to the teeth allergically. Medical treatment involves regular dental cleaning, antibiotics and steroids for pain and inflammation. The disease can occur at any age. Owners will often notice drooling and a decreased appetite. Many cats will have saliva staining on their front feet from rubbing their mouth.
|
|
Selected Conditions:

|
|
|
|

|
|
|
Hepatic Lipidosis
Hepatic lipidosis is liver disease resulting from a period of fasting by the cat. When heavy cats suddenly stop eating the fat in their body is mobilized and causes a & road block in the liver and can lead to liver failure and death. A history of anorexia (stop eating) is often present. Early on many cats will vomit and appear very lethargic. Later signs of lipidosis include the development of jaundice (icterus) which is depicted as bright yellow gums in the photo of the oral cavity seen here. Yellowing can be seen in all mucus membranes, ears, and the whites of the eyes.

|
|
 |
|
Abscess
Abscesses are infections under the skin often due to trauma. The most common cause we see is induced by cats fighting and of course is most common in outdoor cats. The abscess can be anywhere on the body and is seen as a lump that is painful to the touch, hot and is covered in red/inflamed skin. The cat will often have a fever and will be lethargic. Treatment is needed to open and flush the cavity and allow for drainage. Antibiotics are typically used for 10-14 days and the choice may be based on culture of the wound. Most abscesses respond well to treatment.
|
 |
|
|
Urinary Problems
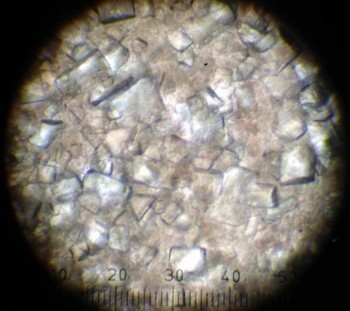
Urinary problems are very common in cats and are often misdiagnosed as behavioral problems when in fact they are often due to infection, stones, inflammation or urinary crystals. A few different types of urinary crystals can occur in cat urine and can be due to a variety of causes. Two common types of crystals are struvites which are often induced by a bacterial infection and oxalates which are thought to have a dietary component. Crystals are actually microscopic precipitation of minerals in the cat’s urine. I often describe these as almost microscopic pieces of glass that the cat must urinate out. It is a very painful condition and the crystals can cause complete blockage in the male cat due to his longer and more narrow urethra. Early on, these cats will often urine mark in the house as they associate the pain of urination with their litter box and therefore attempt to urinate somewhere non-painful. Owners may also notice their cat frequently visiting the litter box and not producing urine or straining. As the cat becomes completely unable to urinate he/she will become ill and lethargic, vomiting and loss of appetite are seen.

Treatment involves relieving the obstruction with an indwelling urinary catheter and flushing fluids through the cat. The urine will be collected and examined for bacteria and crystals and x-rays will often be taken to check for urinary stones. Antibiotics and a diet change are typically required.
|
|
 |
|
BLOOD TESTING: The basics
1. CBC: complete blood cell count – This is a measure of the red blood cells which carry oxygen to the organs, and the white blood cells which are responsible for fighting infection. A CBC will also include information on blood protein and platelets (cells needed for clotting blood). The report will give an estimated count of all the individual cell types in your pet’s blood sample. This will allow your veterinarian to determine information such as:
- Anemia – reduced RBC count
- Increased WBCs – often indicates infection
- Reduced WBCs – can be due to viral infections or stress
- Reduced platelets – can be due to sample handling or an actual reduction for a variety of reasons, very low platelets will place the pet at risk of bleeding, many dogs (greyhounds) will normally have a lower count
- Elevated protein – can indicate dehydration
- Reduced protein – can be due to hemorrhage, lack of production, of loss through the GI tract or kidneys
- Elevated percentage of red blood cells – normal in some breeds such as greyhounds, pet’s living at higher elevations, dehydration
DIAGNOSTICS
Diagnostic testing for animals will vary greatly depending on the age, species, sex and medical condition of the pet. Veterinary medicine has evolved to the point that we are able to provide exceptional quality medical, surgical and diagnostic procedures which allow us to provide the most up to date standard of medical care for your pet. Unfortunately, financial concerns often arise when discussing diagnostic testing and this is most common during an emergency when you are least able to prepare for the additional expense. Because of this, I strongly recommend purchasing pet health insurance. At the very least, insurance will provide you with additional assistance during an emergency, and at the most, it will allow you to provide your pet with life saving care. I’ve provided a few links for pet insurance below and I strongly recommend that all pet owners research the insurance plans available.
It is not possible to cover all types of diagnostic tests available to our pets, but I do intend to include information on the most common diagnostic procedures available and will add additional information over time.
|
|
|
2. Chemistry Panel The blood chemistry panel will provide information on organ status (liver, kidneys, and pancreas), blood protein, immunoglobulins and electrolytes.
3. Thyroid Level (T4): The thyroid level is often added to the chemistry panel for both cats and dogs. While cats often have problems with a thyroid level that is too high, dogs are just the opposite and can have very low thyroid hormone production. A few of the more common signs of hypothyroidism are dry skin, thin hair coat, dry coat, lethargy and weight gain. Dogs with low thyroid levels can be treated with thyroid replacement medication which is inexpensive and safe. For more information on hyperthyroid cats see cat section under links below.
4. In-house Viral/infectious organism testing: These are pre-packaged tests that require the application of blood or urine and positives show various color changes much like a home pregnancy test.
- (dogs) 4DX test: checks for lyme, tick fever (E.canis), anaplasma, and heartworms
- (dogs) Heartworm test: tests only for heartworms
- (cats) FeLV/FIV – Tests for feline leukemia virus and immunodeficiency
- (cats) Feline Combo test – Felv, Fiv, and now heartworms
- (dogs) Parvo Test – tests for parvo virus infections in dogs
URINE TESTING:
1. Urinalysis:A sample is collected from your pet by holding a cup in the urine stream (free catch) or by using a needle directed into the bladder to collect a sterile urine sample. Collection by needle is called cystocentesis and is quick, safe and relatively painless. We prefer to utilize an ultrasound to allow us to see the bladder and actually see the needle enter the bladder, allowing for easier collection.
Information obtained can include:
- Urine Concentration – can indicate kidney disease or dehydration
- Bacteria Count: should be zero when collected by cystocentesis
- RBC – higher with cystocentesis, can indicate inflammation
- WBC count – and bacteria can indicate infection
- Presence and type of urinary crystals
- Presence of glucose (sugar) – can indicate diabetes
- Information regarding liver status – bilirubin
2. Urine Culture and Sensitivity: Urine is collected directly from the bladder by cystocentesis and the sample is plated and incubated in an attempt to grow bacteria. If bacteria are grown, tests are run to indicate the actual type of bacteria and than the bacteria are challenged with various antibiotics to determine the effectiveness of the medications against that specific type of bacteria.
FECAL TESTING: Fecal examinations are commonly done on puppies, kittens and pets with diarrhea.
Routinely used to float parasite eggs to the surface of a liquid where they are collected on a slide coverslip and examined under a microscope. Fecal Direct Smear: Directly plating feces on a slide and examining for moving organisms such as Giardia and smaller ova. Fecal Cytology: Feces are applied to a microscope slide and stained with a dye to allow viewing of cells such as bacteria, RBC and WBC. Fecal cytology can be helpful with diagnosis of gastrointestinal inflammation, microscopic bleeding, and bacterial enteritis.
RADIOGRAPHS:
Commonly called x-rays Allow the veterinarian to see a grey scale image of your pet’s chest, abdomen, and skeletal structures. The size and shape of heart and organs can often be determined and a large amount of useful information can be obtained from radiographs. However, they are not perfect and don’t allow the clinician to see everything. Only structures that are large enough to be seen with the naked eye are seem on x-rays. Many times we will get very poor detail in thin pets or pets with fluid in their abdomen. Also, only the more dense foreign bodies will be seen and items such as cloth will not be seen at all.
Advantages:
- Readily available in most veterinary hospitals
- Can often provide a quick in house diagnosis
- Excellent for viewing skeletal structures
- Can often provide supportive information to help confirm a diagnosis
Disadvantages:
- Viewing in shades of gray and is not the same as actually seeing the structures
- Abdominal detail is influenced by the degree of fat and reduced by fluid
- Only structures large enough to be seen with the naked eye will show up
- Biopsy is often needed for a more specific diagnosis of organ disease
ULTRASONOGRAPHY:
The same as a pregnancy ultrasound but also used for viewing structures in the abdomen and the thorax (chest). An ultrasound of the heart is called an echocardiogram and is an excellent tool for diagnosing the type and severity of heart disease. Abdominal ultrasounds can be used for those pets that have poor abdominal detail on radiographs or for a guided biopsy of organs or a mass.
ENDOSCOPY:
A long flexible or rigid tube made of mirrors that allow the veterinarian to actually view the interior of the patient. The endoscope can be inserted into just about an area of the body and small biopsy samples can be taken or foreign bodies (i.e. fish hooks) collected.
Advantages:
- Allows a direct view of internal structures
- Allows for possibility of a quick and non-surgical diagnosis
- Allows for a non-surgical biopsy
- Can collect photos or videos of internal structures for later review
Disadvantages:
- Limited by the size of the tube, very small scopes needed for some areas
- Can only collect small and often superficial biopsy samples
- Often able to make a diagnosis but surgery may still be needed for cure
ECG or EKG:
Leads are attached to the body and measure the electrical activity of the heart. Information on heart rate and rhythm is collected.
|
|

|
BLOOD PRESSURE:
It is vitally important that this be measured while a pet is under anesthesia A frequently used tool in older cats suspected of having hyperthyroidism or heart disease. Or in dogs with conditions such as Cushings. Blood pressure cuffs come in different sizes and it is important to select the correct size for the patient. The width of the cuff needs to be about 0.3-0.4 times the diameter of the limb. To quickly check the fit of the cuff align the cuff with the limb lengthwise and the cuff should go less than half way around the limb diameter and at least a quarter of the diameter. A cuff size that is too wide will result in a lowered blood pressure reading.
We also like to place the pet in a darkened room on a comfy bed and have the owners talk to the pet while we are measuring the blood pressure. All these procedures help to calm the pet and result in more accurate readings. Regular blood pressure measurements can be useful for cats with kidney disease and hyperthyroidism.
|
|

|
ANESTHESIA
Many people are concerned about anesthesia and allow this concern to prevent their pet from getting needed treatments and diagnostics. While there is always some risk with any general anesthetic procedure, there are many things both you and your veterinarian can do to dramatically lessen the risk.
What you can do: You are your pet’s advocate and are directly responsible for making decisions to provide your pet with a safer anesthetic procedure. Some of these decisions include:
- Choosing to have the procedure preformed with your regular veterinarian rather than the low cost clinic down the road. This is important for a few reasons, but most importantly is that your doctor knows your pet and therefore is better able to predict potential problems and pick the best anesthetic protocol for your pet. Additionally, while many low-cost clinics practice excellent medicine, unfortunately some are able to provide lower cost because they cut corners in other ways such as less expensive anesthetic gas, few injectable anesthetics, less pain control, reduced staffing and less (or no) monitoring of the pet under anesthesia.
- Choosing to have pre-anesthetic blood work completed on your pet. Some hospitals will require that pre-anesthetic blood work be completed on all pets, some will only require it on geriatric (senior) pets, and some will leave the decision entirely up to you. Pre-anesthetic blood work provides the veterinarian with a picture of the health of your pet at the time of the procedure. The picture includes information on general organ status, potential infections, ability to clot blood, and anemia. Frequent problems identified include diabetes, liver disease, kidney disease and clues to infections or parasites. Young pets are generally assumed to be healthy and therefore owners often elect to forgo blood testing. Most of the time this is a relatively safe bet, but it is a gamble and occasionally even a young pet will have unidentified disease that will increase the anesthetic risk. If disease is identified the anesthesia may be postponed or the anesthetic protocol may be altered to increase the margin of safety for your pet. When asked to choose pre-anesthetic blood work for your pet, always ask yourself if you would want this checked on you prior to surgery.
- Choosing to have an IV catheter placed and have your pet maintained on IV fluids Again, many hospitals require the pet be placed on IV fluids during the procedure, but you may be asked to make this decision for your pet at some hospitals. An IV catheter provides an immediate entry to a vein in the case of an anesthetic emergency and allows for the immediate administration of potentially life saving medications. Additionally, the catheter allows for the administration of IV fluids which support the pet’s blood pressure during general anesthesia and this helps to keep good blood flow to the kidneys which is important for all pets, but essential for those pets with early kidney disease.
- Allowing for safer types of anesthetics recommended by your veterinarian.
We are fortunate in veterinary medicine to have a large variety of anesthetics available to us which allows us to choose the safest anesthetic for your pet. As an example, some anesthetics are just inhaled and others are injectable. Often a combination of the two is used. Even the injectable drugs have large differences between them that can alter the safety of the procedure. Some anesthetics cause longer periods of anesthetic before the pet can awaken, some cause much more suppression on heart function and respiration, some have more of an affect on the liver or kidneys, and some shouldn’t be used in particular breeds of animals at all. At the time of this writing one of the safest and most adjustable anesthetic gasses is Sevoflurane. It is considered a human grade anesthetic gas and allows for very rapid changes in anesthetic depths.
Many times, if the veterinarian determines that your pet needs a specific type of drug it will just be implemented. However, occasionally a specific anesthetic will result in a higher expense and again you may be asked to make a decision depending upon the hospital olicy. Your veterinarian should always explain why a particular drug is recommended and provide you with the correct facts to help with the decision.
|
|

|
What Your Veterinarian Can Do: Your veterinarian is ultimately responsible for the safety of your pet under anesthesia and will be able to ensure the safety in many ways.
Physical Exam and history Your veterinarian will read through your pet’s medical chart to help determine the health status and any existing potential anesthetic problems or allergies. A complete physical exam will be done on all pets prior to anesthesia to again look for potential disease problems which may alter the anesthetic protocol needed. As an example, short nosed breeds of dogs (pugs) & cats (Persians) will have a delayed extubation which means that the breathing tube will be kept in the pet as long as possible when the anesthetic gas is shut off and the pet is maintained on oxygen. Brachycephalic or short nosed breeds are likely to have more problems breathing when awakening from anesthesia and delayed extubation resolves those problems by providing an open airway until the pet is more awake and better able to breathe normally.
Anesthetic choices Veterinarians have various means of providing general anesthesia for your pet and this allows us to determine the safest choices for him/her.
The choices can include:
- Using gas anesthesia to induce (cause the pet to sleep) the pet vs. using injectable anesthesia to induce the pet.
- Injectable induction is the most common method and is the fastest and easiest on your pet.
- Pets with liver or kidney disease may be induced with gas alone via a mask or an induction box. Pets maintained on gas alone will awaken quickly, but also take a little longer to induce and their blood pressure must be monitored very carefully.
Types of injectable anesthetics used Again, there are many choices here as well. At our hospital we typically will induce with telazole or a combination of ketamine and valuim. These both have proven very safe for us and have minimal suppressive effects on cardiovascular or respiratory function.
- For very short anesthetic procedures in which we would like the pet to be able to go home quickly, or for geriatric pets with organ disease, we will often use a drug called Propofol. This anesthetic is very safe and extremely short acting. Pets will typically awaken fully in 5-10 minutes and they awaken easily as if they had just been snoozing.
- Other injectable anesthetics include those that provide a combination of pain relief and anesthesia and allow for reversal of the anesthesia with a second injection. These can have some suppression of blood pressure and are only reserved for young healthy pets undergoing very short procedures.
Types of anesthetic gasses used Once again, veterinarians have the ability to choose the type of anesthetic gas used on your pet. Some of the older anesthetic gasses are much less expensive but also can cause problems in older pets, can result in liver disease and cause slower changes when the pet’s level of anesthesia needs to be adjusted. An example of an older type of anesthetic gas is halothane. The newer and of course more expensive anesthetic gasses include isoflurane and sevoflurane. These gasses are extremely safe and are commonly used in geriatric pets. They also provide the ability to quickly change the depth of anesthesia. I recommend using only one of these gasses.
Monitoring (really the MOST important aspect) Monitoring of your pet’s vitals (depth of anesthesia, respiration, temperature, heart rate, blood oxygen saturation, blood pressure) should be done by one designated individual throughout the procedure and the results should be recorded throughout the procedure. Monitoring allows the person performing the procedure to focus on completing the procedure to the best of their abilities without dividing their attention between the task at and and anesthetic monitoring. Good monitoring also allows for the correct level of anesthesia to be chosen throughout the procedure. Most hospitals will provide some way of monitoring your pet, but the way the pet is monitored and the values monitored may vary depending upon the equipment and the staff available.
Recovery from anesthesia The recovery or awakening period is just as important as the actual anesthetic procedure. The pet should be closely monitored during this time, the temperature should be taken and warmth should be provided if needed, the pet should have delayed extubation if needed and the pet should be supervised until fully awake.
for more information on pain control read below…
|
|

|
PAIN CONTROL IN COMPANION ANIMALS
Research has shown that pain is self perpetuating and that each episode of pain triggers the next, making it easier to experience the pain. Therefore, after the animal begins to experience pain it is much more difficult to control because the pet is already cycling through this pain loop. Additionally, research studies indicate that pain will not only cause the animal stress but that the stress will release steroids which will delay healing and recovery.
Interpretation of pain in the various animals we care for can be extremely problematic. In the veterinary field we not only deal with various animal personalities but also various species that show pain differently. As an example, a budgie that is painful will often just sit quietly and appear slightly fluffed, but a Husky will often vocalize at the smallest pain stimulation. Animals, like people, have various levels of pain sensitivity and some animals will be very vocal with minimal pain stimulation whereas others will never show pain sensitivity even though we know they are experiencing a painful condition.
Because of the difficulty of interpreting pain in various animals/species and because of the difficulty of halting pain once it has begun, veterinarians, as your pet’s health care provider, must control pain before it starts. We know if certain procedures are likely to cause pain and we can administer pain control prior to the procedure to prevent the pet from 1) experiencing the pain, & 2) entering the difficult to control pain cycle.
The importance of multi-modality pain control should also be addressed. We are fortunate to have a large spectrum of analgesics (pain medications) available to us in the veterinary field, and by combining different types of analgesics we can often get additive effects, where the combination of drugs work better together than either one alone. A good example of this is the use of a non-steroidal anti-inflammatory drug (NSAID) and a true analgesic such as a morphine derivative. The NSAID will eliminate the swelling and the morphine derivative will directly control the pain providing a broader spectrum of pain control.
In conclusion, veterinarians understand that animals do experience pain much like we do, but the presence of pain and its control are subjective and difficult to interpret. Therefore, my ideal pain control involves the administration of analgesics prior to a painful event and the prevention of any discomfort. Veterinary medicine of the past poorly understood this concept and approved drugs were not available, however, veterinary medicine has changed and today pain control is an important part of our acceptable standard of care for your pet
|
 |
LINKS:
One of the best web sites providing owners with information about specific disease states is veterinary partners
American Animal Hospital Association Pet library
CATS
Feline Hypertrophic Cardiomyopathy
Chronic Renal (kidney) Failure
Vet info for CAT owners page
Gastrointestinal Parasites of Cats – Cornell
Aging Chart
Gastrointestinal Parasites of Cats – Cornell/ for pet owners
The Cat Site.com – everything cats including behavior
Feline Grooming Disorders and Obsessive Compulsive disorder
|
|